
- 07914803818
- 02077940500 ext: 34273
- mvarcada.practice@nhs.net

INTRODUCTION — PR bleeding is defined as Rectal passage of minimal bright red blood most commonly occurs in a chronic intermittent pattern with or without pain. The term bright red (fresh) blood per rectum is used to indicate small amounts of red blood on toilet paper after wiping or a few drops of blood in the toilet bowl after defecation.
Benign causes are common and account for 90 percent or more of all episodes of fresh PR bleeding. The true proportion of benign etiologies may be even higher, since many young people with minimal PR bleeding never present for care. However, scant rectal bleeding is also a common presenting symptom of serious diagnoses, such as colorectal cancer
DIFFERENTIAL DIAGNOSIS — The causes of bright red blood per rectum are different and depends on different factor like age, medication diet, lifestyle. Only when a lesion is witnessed to be actively bleeding can it be definitively considered the cause of bleeding.
Common causes and presentations of PR Bleeding include:
Haemorrhoids
Anal fissures
Polyps
Proctitis
Rectal ulcers
Cancer
Diverticulosis is a common finding on endoscopy in older adults but is generally an incidental finding in the workup of chronic PR bleeding, since diverticular bleeding is usually more acute and of greater volume.
OPC and CLINICAL ASSESSMENT:
History: directed at confirming the diagnosis of Fresh rectal bleeding and at identifying potentially worrisome symptoms and risk factors
Physical examination : A detailed physical examination must include external inspection of the anus and a digital rectal examination. An Out Patient Clinic anoscopy or proctoscopy should be carried out in patients who present with acute minimal bleeding because these are simple maneuvers that do not require bowel preparation and with high sensitivity
Laboratory testing: A complete blood count (FBC) and ferritin are reasonable preliminary tests in patients over age 40, or those with other risk factors for colonic neoplasia, such as family history
Sigmoidoscopy versus colonoscopy — Flexible sigmoidoscopy investigates 60 cm of the colon It has the advantages over colonoscopy that it can be done without sedation (although sedation is sometimes used for the procedure) The main disadvantage of sigmoidoscopy is the potential need for a colonoscopy if a source of bleeding is not found or if a distal adenomatous polyp is found, thus exposing the patient to two endoscopic procedures.
Colonoscopy is the definitive tool for evaluating the entire colon for neoplastic lesions and is also a sensitive tool for the detection of all other bleeding lesions in the lower gastrointestinal tract Colonoscopy requires full bowel preparation and a facility where the test is available. It is often performed under conscious sedation.
Treatment: (also see One Stop Clinic).
Treatment depends on diagnosis and severe of symptoms and need to be discussed with your Colorectal Consultant once diagnosis confirmed. Majority of treatment can be performed in Out patient clinic or under ambulatory regime.
Red flags: Patients with minimal PR bleeding in the following categories should undergo additional testing regardless of age:
Colonic polyps, also known as colorectal polyps, are growths that appear on the surface of the colon. The colon, or large intestine, is a long hollow tube at the bottom of the digestive tract. It’s where the body makes and stores stool.
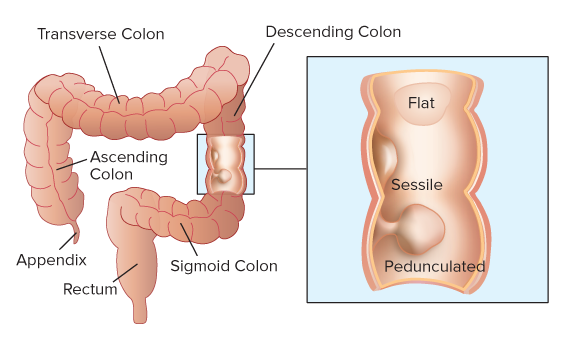
Polyps in the colon can vary in size and number. There are three types of colon polyps:
Hyperplastic polyps are harmless and do not develop into cancer.
Adenomatous polyps are the most common. Although most will never develop into cancer, they do have the potential to develop into colon cancer.
Malignant polyps are polyps that are noted under microscopic examination to have cancer cells in them.
In most cases, polyps do not cause symptoms and are usually found on routine colon cancer screening exams. However, if you do experience symptoms, they may include:
blood in the stool or rectal bleeding
pain, diarrhea, or constipation that lasts longer than one week
nausea or vomiting if you have a large polyp
Blood on your toilet tissue or blood streaked stools may be an indication of rectal bleeding and should be evaluated by a doctor.
It's important to have regular screening tests to detect any existing polyps. When colonic polyps are found in the early stages, they can often be removed safely and completely during a colonoscopy. Removing polyps may reduce your risk of developing colon cancer.
Doctors don’t know the exact cause of colonic polyps, but polyps result from abnormal tissue growth. The body periodically develops new healthy cells to replace old cells that are damaged or no longer needed. The growth and division of new cells is usually regulated. In some cases, however, new cells grow and divide before they’re needed. This excess growth causes polyps to form. The polyps can develop in any area of the colon.
Colonoscopy: During this procedure, a camera attached to a thin, flexible tube is threaded through the anus. This allows your doctor to view the rectum and colon. If a polyp is found, your doctor can remove it immediately or take tissue samples for analysis.
Sigmoidoscopy: This screening method is similar to a colonoscopy, but it can only be used to see the rectum and lower colon. It can’t be used to take a biopsy, or a sample of tissue. If your doctor detects a polyp, you'll need to schedule a colonoscopy to have it removed.
Barium enema: For this test, your doctor injects liquid barium into your rectum and then uses a special X-ray to take images of your colon. Barium makes your colon appear white in the pictures. Since polyps are dark, they’re easy to identify against the white color.
CT colonography: This procedure uses a CT scan to construct images of the colon and rectum. After the scan, a computer combines the images of the colon and rectum to produce both 2- and 3-D views of the area. A CT colonography is sometimes called a virtual colonoscopy. It can show swollen tissues, masses, ulcers, and polyps.
Stool test: Your doctor will give you a test kit and instructions for providing a stool sample. You’ll return the sample to your doctor’s office for analysis, especially to test for microscopic bleeding. This test will show if you have blood in your stool, which can be a sign of a polyp.
The best way to treat colonic polyps is to remove them. Your doctor will likely remove your polyps during a colonoscopy. The polyps are then examined under the microscope to see what type of polyp it is and if there are any cancer cells present. Doctors can usually get rid of polyps without performing surgery.
However, you may need surgery to remove the polyps if they’re large and can’t be removed during a colonoscopy. In most cases, this can be done by laparoscopic surgery. This type of surgery is minimally invasive and uses an instrument called a laparoscope. A laparoscope is a long, thin tube with a high-intensity light and a high-resolution camera at the front. The instrument is inserted through an incision in the abdomen. Once your surgeon has a visual of your colon, they’ll remove the polyps using a special tool.
A pathologist, or someone who specializes in tissue analysis, will check the polyps for cancerous cells.
Adenoma is a type of non-cancerous tumor or benign that may affect various organs. It is derived from the word “adeno” meaning 'pertaining to a gland'.
Every cell in the body has a tightly regulated system that dictates when it needs to grow, mature and eventually die off. Tumors and cancers occur when cells lose this control and divide and proliferate indiscriminately.
The basic difference between a benign tumor and a cancer is its slower growth and lower capacity to spread. In other words adenomas are much less aggressive in terms of growth than adenocarcinomas.
Adenomas may affect various organs including Colon, Pituitary gland, Thyroid gland, Breasts, Adrenal gland and Kidneys.
Colons are the most common organs that are affected by adenomas. There may be detected on colonoscopy. A regular surveillance of colonic adenomas and preferable removal of these tumors is advised as they have a very high potential to become colon cancers.
Neuroendocrine tumours (NETs) are rare tumours that can occur in the cells of the neuroendocrine system.
The neuroendocrine system consists of nerve and gland cells. It produces hormones and releases them into the bloodstream.
NETs are tumours (abnormal growths) that develop in the cells of the neuroendocrine system.
NETs can be malignant (cancerous) or benign (non-cancerous) and often – but not always – grow slowly. There are a number of different types of NET, depending on the specific cells affected.
Gastroenteropancreatic neuroendocrine tumours (GEP NETs) are tumours that develop in the gut or pancreas.
Gastrointestinal neuroendocrine tumours (GI NETs) develop in the digestive system, which includes the bowel, stomach or oesophagus. Pancreatic neuroendocrine tumours (pNETs) develop in the pancreas.
Pulmonary neuroendocrine tumours develop in the lungs. Rarely, NETs can also develop in other parts of the body, including in the liver, gallbladder, bile ducts, kidneys, ovaries, or testicles.
Some NETs, known as functioning tumours, produce hormones that cause specific symptoms. Tumours that don't cause symptoms are known as non-functioning tumours.
The symptoms of a neuroendocrine tumour can vary depending on where it is and what hormones it produces.
For example, a tumour in the digestive system may cause diarrhoea, constipation or tummy pains. A tumour in the lung may cause wheezing or a persistent cough.
Some tumours (functioning tumours) may cause abnormally large amounts of hormones to be released into the bloodstream.
This can cause symptoms such as diarrhoea, flushing, cramps, wheezing, low blood sugar (hypoglycaemia), changes in blood pressure and heart problems.
What causes neuroendocrine tumours isn't fully understood. However, your chance of developing an NET is increased if you have one of the following rare conditions or syndromes:
multiple endocrine neoplasia type 1 (MEN 1) – a rare inherited condition where tumours in the endocrine system develop, most commonly in the parathyroid glands, pituitary gland and the pancreas
neurofibrmatosis type 1 – a group of genetic conditions that cause tumours to grow along your nerves
Von Hippel-Lindau syndrome (VHL) – an inherited condition that causes blood vessels to grow abnormally
Research has also shown that your risk of developing an NET is slightly increased if one of your parents has had one in the past.
There are many tests that can be used to diagnose NETs, including blood tests, urine tests, scans, and a biopsy (where a small tissue sample is taken for closer examination).
Different types of scans may also be used to identify or examine tumours. These include:
ultrasound scans – including echocardiograms and endoscopic ultrasound scans
computerised tomography (CT) scans
magnetic resonance imaging (MRI) scans
positron emission tomography (PET) scans
octreotide scans – where mild radioactive liquid is injected into your veins and a special camera is used to highlight any cancerous cells.
How a neuroendocrine tumour is treated will depend on your individual circumstances. For example, your treatment will depend on:
Unfortunately, many people are only diagnosed after other parts of their body are affected. However, it may still be possible to surgically remove the tumour, even if it has spread to other parts of your body. If surgery can't be used to completely cure your condition, it may be used to help manage and reduce any symptoms that you have.
It may also be possible to shrink the tumour or stop further growth using treatments that block the blood supply to the tumour (embolisation), or chemotherapy, radiotherapy or radiofrequency ablation (where heat is used to destroy the cells).
Source : http://www.nhs.uk/
Pelvic cancer refers to a variety of cancers involving the structures and organs in the pelvis. Your pelvic area is the lower portion of the trunk of your body. It contains the pelvic bones, bladder, rectum, and reproductive organs.
Pelvic cancers that can affect both sexes include bladder cancer, anal cancer, rectal cancer, chondrosarcoma (cancer of the cartilage), and osteosarcoma (cancer of the bone). Pelvic cancer can also occur from the spread or metastasis of other cancers from different areas of the body.
Because the pelvic area contains the reproductive organs, there are pelvic cancers that can affect men and women separately. For men, this includes prostate and testicular cancer. For women, pelvic cancer can include cervical, ovarian, uterine or endometrial, vaginal, and vulvar cancer.
Normally, old or damaged cells in your body will stop dividing and die before they can become cancerous. Healthy young cells usually replace these cells. Cancer occurs when old or damaged cells continue to divide and multiply uncontrollably. In pelvic cancer, the malignancy or cancer develops in the structures or organs of the pelvic area.
Treatment and prognosis of pelvic cancer varies depending on the type of cancer and the stage of advancement; your age, medical history, and coexisting conditions or diseases; and other factors. Treatment may include surgery, radiation therapy, hormone therapy, and chemotherapy. In general, diagnosis and treatment in an early stage of development, before cancer cells have spread, offers the best prognosis for a complete cure.
Pelvic cancer can lead to life-threatening complications and can be fatal, especially left undetected and untreated. Seeking regular medical care offers the best chances of discovering pelvic cancer in its earliest, most curable stage, often before symptoms are present. If you have pelvic cancer, following your treatment plan may help reduce your risk of serious complications.
Anal cancer is a malignancy of the anus, which is the opening that allows the passage of stool. Rectal cancer is a malignancy of the rectum, the final portion of the large intestine that holds stool for elimination. Symptoms of anal and rectal cancer may include:
Normally cells in your body that are old or damaged will stop dividing and die before they can become cancerous. Healthy young cells usually replace these cells. Pelvic cancer occurs when old or damaged cells to continue to divide and multiply uncontrollably. What causes this to happen is not known for most cancers.
Some cancers have more definite causes. For example, certain types of cancers, such as ovarian cancer, have been linked to mutations of specific genes. Cervical cancer is an example of a cancer that is most often caused by a human papillomavirus (HPV) infection. HPV, which can also cause genital warts, is spread through sexual contact and often has no symptoms. HPV has also been linked to vaginal, vulvar and anal cancer.
Treatment of pelvic cancer begins with seeking regular, routine medical care throughout your life. Regular medical care allows your healthcare provider to best evaluate your risks of developing pelvic cancer and perform routine screening measures, diagnostic testing, and other assessments as needed. These measures greatly increase the chances of detecting pelvic cancer in its earliest, most curable stage.
The goal of pelvic cancer treatment is to permanently cure the cancer or to bring about a complete remission of the disease. Remission means that there is no longer any sign of the disease in your body, although it may recur or relapse later. Pelvic cancer treatment plans use a multifaceted approach. They are individualized based on the type and stage of the disease, your age, your medical history, and any coexisting diseases or conditions.
Crohn's disease is a chronic inflammatory bowel disease. Inflammatory means that the body's own immune system is attacking the digestive tract anywhere from the mouth to the anus, though usually it attacks areas in the small and large intestines. It usually develops in the late teens/early 20s or in the 50-60 age group. If managed, the disease can be controlled and hopefully prevented from relapsing, though there is currently no cure.
What causes Crohn's?
There is no known single definitive cause for Crohn's disease. As far as we currently know, it is caused by an interaction between your genes, the environment, your lifestyle (eg. smoking) and natural variants in your immune system. Research is still ongoing into finding more answers.
What complications are there?
As Crohn's is a chronic condition, a relapse may happen at any point. This may be evident with a return to your original symptoms, which may include diarrhoea, abdominal pain, weight loss, loss of appetite, and even blood in your stools. You will need to see your GP if you have a relapse. Crohn's can also affect areas other than the digestive tract. You may get sore, red eyes, painful joints, and unusual rashes on your skin. In addition, the disease can cause complications in and around the anus. You can get something called a fissure, which is a crack in the skin around the anus, which can bleed. You may also develop fistulae, which are abnormal connections between the digestive tract and the outside. Although unpleasant, these can be treated. Abscesses and piles may also develop.
How is Crohn's disease treated?
There are two goals to managing Crohn's disease. First the disease is brought under control so it doesn't affect you as much (inducing remission) and then you aim to keep it that way (maintaining remission). One of the most important things to do is stop smoking. Services to assist this are available at your GP or at your hospital.
Inducing remission: To bring Crohn's under control after a flare, or when first seen by a doctor, a steroid will be used, usually in tablet form, but possibly by a drip into your veins. Side effects of this treatment can include acne and mood changes, but these will not be permanent as you will be slowly taken off the steroid. There may be an option for surgical removal of the bowel however this is not a cure.
Maintaining remission: To keep your disease under control, there are a variety of options that your doctor will discuss with you. Most people will be on either Mercaptopurine or Azathioprine. It is important to carry on taking these if you start, as stopping increases the chances of relapse. Other drugs, such as Infliximab, are available, though not usually the first choice treatment. If you have had surgery then your doctor may suggest that you take one of the above drugs. Even if you choose not to receive treatment, your doctor will continue with check-ups and monitor your disease.
Crohn's disease and Cancer Another type of inflammatory bowel disease, Ulcerative Colitis, is associated with an increased risk of bowel cancer. However, as Crohn's can affect all over the digestive tract, the risk of cancer varies. If your small bowel is mainly affected, then it is unlikely to increase your risk of cancer. If it affects the large intestine extensively, often called Crohn's colitis, then the risk increases after 20 years of disease to 7 in 100 people (compared to 5 in 100 of the general population).
Crohn's and Pregnancy It is important that you talk to your doctor if you are hoping to conceive. Many people with Crohn's have gone on to have healthy children, but there are important things to consider. One of these for women is that if your disease is active, it may be harder to conceive. Most doctors will advise having your disease under control before trying to conceive, as it can complicate pregnancy. Some medications may also have side effects upon your baby, so it is best to discuss this with your doctor.
Ulcerative colitis is an intermittent form of inflammatory bowel disease affecting the rectum and often extending into the colon. It is currently thought that usually harmless bacteria can cause a reaction in certain individuals, leading to their colon becoming inflamed. The reason this affects some people but not others is not fully understood.
Who does ulcerative colitis affect?
Ulcerative colitis usually begins between 15 and 30 years of age, and it can affect men and women equally. Approximately 100,000 people in the UK are affected by ulcerative colitis.
What are the symptoms?
The three most common symptoms are: diarrhoea bleeding from the back passage abdominal pain Not everyone will experience all three symptoms at once; for example some patients may only notice they pass blood when opening their bowels. Patients may also experience some weight loss and fevers. Occasionally the inflammation in ulcerative colitis can affect other parts of the body, such as the joints or skin.
What is a colonoscopy and why do I need one?
A colonoscopy is an examination with a camera on a flexible tube that is inserted into the back passage, usually you are sedated. With this it is possible to see the rectum and the entire colon.
Your doctor may take a few biopsies during this procedure (small samples of the bowel lining). With this it is possible to diagnose ulcerative colitis as well as seeing the extent of disease. Individuals with long-term ulcerative colitis are also at a slightly increased risk of bowel cancer, so a colonoscopy can be performed to look for any early signs of disease.
What treatment options are available?
Anti-inflammatory medication may come as a suppository or as tablets. Although suppositories may seem unpleasant, they ensure the medication gets directly to the site of disease and are useful when only a small amount of the colon is affected. If the inflammation is severe, you may be given steroids. These are reserved for severe cases because they come with more side effects.
Some anti-inflammatory treatments are also given when the disease is inactive to prevent relapse.
What if medication fails?
If ulcerative colitis fails to respond to treatment, or patients become very unwell, a surgical operation to remove some or the entire colon is considered, called a colectomy.
Removal of the colon prevents it becoming inflamed, so treats the disease. This procedure previously required the patient to need a colostomy bag on their abdomen, but instead nowadays part of the small intestine can usually be made into a pouch which acts as the rectum, meaning a colostomy bag is not needed.
Microscopic colitis is a condition that causes watery diarrhea. It involves the colon, which is another name for the large intestine. There are 2 types of microscopic colitis, lymphocytic colitis and collagenous colitis. Both types cause the same symptoms and are treated the same way.
Who gets microscopic colitis?
Microscopic colitis happens when the colon gets inflamed. But doctors don't always know what makes the colon inflamed. In some cases, the condition seems to be caused by an infection in the digestive system. In other cases, it seems to be caused by medicines. For example, a group of medicines called non-steroidal antiinflammatory drugs, or "NSAIDs" for short, sometimes causes microscopic colitis.
What are the symptoms of microscopic colitis?
Microscopic colitis causes episodes of diarrhoea that is watery and not bloody. Most people have 4 to 9 watery bowel movements a day, but some people have more. Diarrhoea can last weeks to months.
People sometimes have other symptoms, too. These commonly include weight loss, belly pain, or feeling very tired.
Test for microscopic colitis:
Your doctor or nurse will do an exam and order different tests to exclude other causes of diarrhoea and diagnose microscopic colitis. These can include:
- Blood tests
- Lab tests on a sample of your bowel movement
Colonoscopy – This is a procedure that lets the doctor look at the inside of your colon. During a colonoscopy, the doctor will do a test called a biopsy and he will take small samples of tissue from your colon. A biopsy is the only test that can tell for sure whether you have microscopic colitis.
Treatment
Treatment depends on your individual situation. It usually involves one or more of the following:
Medicine changes – If your doctor thinks that your symptoms are caused by a medicine you take, he or she will recommend that you stop taking that medicine.
Anti-diarrhoea medicines, such as loperamide (brand name: Imodium) These medicines reduce the number of bowel movements you have.
A steroid medicine called budesonide. This is different from the steroids athletes take to build muscle. This medicine helps reduce inflammation in the colon.
If these treatments don't help enough to ease your symptoms, let your doctor or nurse know. There are other medicines or treatments that might help.
Some people need to be on treatment long term. That's because symptoms sometimes come back after treatment is stopped.
High likelihood |
Intermediate likelihood |
Low likelihood |
Acarbose |
Carbamazepine |
Cimetidine |
Aspirin and NSAIDs |
Celecoxib |
Gold salts |
Clozapine |
Duloxetine |
Piascledine |
Entocapone |
Fluvastatin |
|
Flavonoid* |
Flutamide |
|
Proton pump inhibitors |
Oxetorone |
|
Ranitidine |
Madopar |
|
Sertraline |
Paroxetine |
|
Ticlopidine |
Simvastatin |
|
A functional gastrointestinal disorder comprises symptoms arising in the mid or lower gastrointestinal tract that are not attributable to anatomic or biochemical defects. The symptoms include abdominal pain, early satiety, nausea, bloating, distention, and various symptoms of disordered defecation. The three most common functional bowel disorders are irritable bowel syndrome (IBS), constipation, and functional dyspepsia.
IBS, the most common functional bowel disorder, is characterized by chronic or recurrent symptoms of lower abdominal pain related to bowel movements, change in bowel habit (diarrhoea, constipation, or alternating), a sense of incomplete rectal evacuation, passage of mucus with stool, and abdominal bloating and distention.
Functional dyspepsia is characterized by chronic or recurrent pain or discomfort centered in the upper abdomen. Unlike IBS, symptoms are not related to the process of defecation. There is no evidence of organic disease or structural or biochemical abnormality.
Constipation is where you have one or more of the following:
Constipation is very common in the UK, with up to four in 10 people affected. It is normal to be embarrassed to talk about constipation, but there are many ways to treat it and if treated it has no long-term effects on health in most people.
How often should I be emptying my bowels?What is normal for one person is not necessarily normal for another. Some people may empty their bowels three times a day, whilst for others once every three days may be normal. If you are emptying your bowels less often than you normally do, then you may be constipated.
Why are healthy bowel motions important?
Maintaining your own regular bowel motions is important for preventing the complications that constipation can bring. If you do not treat your constipation and it continues for a long time, you may develop haemorrhoids (dilated blood vessels around your anus from straining too hard) or faecal impaction (stools so hard that they collect in your rectum and cannot be passed)
What causes constipation?
There are many causes of constipation. The common ones include:
How is constipation treated?
The first treatment for constipation is to change the food you eat and increase the amount of water you drink in a day (see below). Exercise helps treat constipation by using gravity to help the food along the gut.
If the above do not work, your doctor may prescribe laxatives.
Faecal impaction may be treated by your doctor inserting a gloved finger into the rectum and manually breaking the stool up so that it can be passed.
How can I prevent constipation?
As with most medical conditions, prevention is better than cure. The key to preventing constipation is eating the right kinds of food and drinking enough water to keep your stools bulky and soft enough to pass through your gut easily. Use the tick boxes to check off the measures you have taken to prevent constipation:
What is bowel incontinence?
Bowel incontinence occurs when you are unable to voluntarily control bowel movements, leading to leakage from the back passage. This very common condition can be upsetting; however there are a wide variety of treatments available to help.
What causes bowel incontinence?
Bowel incontinence is not a single disease in itself; it has a wide variety of causes. The main ones are as follows:Many of these conditions are more common in the elderly, although bowel incontinence itself is not a normal part of ageing.
This condition is more common in women than men because it can develop as a complication of childbirth.
What are the symptoms of bowel incontinence?
A sudden urge to go to open your bowels and not being able to reach the lavatory in time (urge incontinence).
The passing of stool without knowing it (passive soiling).
Passing stool inadvertently while passing wind.
Symptoms may be experienced differently by different people and are not necessarily present all of the time. Some of the associated symptoms include:
How is bowel incontinence diagnosed?
Your GP will normally be able to make the diagnosis after you tell him/her your symptoms.
To investigate the cause your doctor may insert a gloved finger into your rectum to check for impacted stools and test the power of the anal sphincter muscles.
What other tests might be useful?
What treatments are available?
As a rule the least invasive and most agreeable solution will be considered first. Bowel incontinence is not uncommon and treatment is widely available.
What is a hernia? — Your internal organs and tissues are held in place by a tough outer wall of tissue called the “abdominal wall.” An abdominal hernia is an area in that wall that is weak or torn. Often when there is a hernia, organs or tissues that are normally held in place by the abdominal wall bulge or stick out through the weak or torn spot.
There are many different kinds of abdominal wall hernias:
What are the symptoms of abdominal wall hernias? — Abdominal wall hernias do not always cause symptoms. When they do, they can cause some or all of these symptoms:
A bulge somewhere on the trunk of the body – This bulge can be so small that you don’t even realize it’s there.
Pain, especially when coughing, straining, or using nearby muscles
A pulling sensation around the bulge
Abdominal wall hernias can balloon out and form a sac. That sac can end up holding a loop of intestine or a piece of fat that should normally be tucked inside the belly. This can be painful and even dangerous if the tissue in the hernia gets trapped and unable to slide back into the belly. When this happens, the tissue does not get enough blood, so it can become swollen or even die.
Should I see a doctor? — Yes. See a doctor if you have any of the symptoms of a hernia. In most cases, doctors can diagnose a hernia just by doing an exam. During the exam, the doctor might ask you to cough or bear down while pressing on your hernia. This might be uncomfortable, but it is necessary to find the source of the problem.
Most of the time, the contents of the hernia can be “reduced,” or gently pushed back into the belly. Still, there are times when the hernia gets trapped and won’t go back in. If that happens, the tissue that is trapped can get damaged.
If you develop pain around a hernia bulge or feel sick, call your doctor or surgeon right away.
How are hernias treated? — Not all hernias need treatment right away. But many do need to be repaired with surgery. Surgeons can repair most hernias in 1 of 2 ways. The right surgery for you will depend on the size of your hernia, where on the abdominal wall it is, whether this is the first time it is getting repaired, and what your general health is like. The types of surgery are:
Open surgery – During an open surgery, the surgeon makes an incision near the hernia. Then he or she looks at the tissue that is stuck in the hernia, and if it is healthy, gently pushes it back into place. Sometimes a piece of tissue needs to be removed. Next, the surgeon sews the layers of the abdominal wall back together, so that nothing can bulge through. In some cases, surgeons will also patch the area with a piece of mesh. The mesh takes some of the strain off the abdominal wall. That way the hernia is less likely to happen again.
Laparoscopic surgery– During laparoscopic surgery, the surgeon makes a few incisions that are much smaller than those used in open surgery. Then he or she inserts long thin tools into the area near the hernia. One of the tools has a camera (called a “laparoscope”) on the end, which sends pictures to a TV screen. The surgeon can look at the picture on the screen to guide his or her movements. Then he or she uses the long tools to repair the hernia using mesh.
If your hernia has reduced the blood supply to a loop of intestine, your doctor might need to remove that piece of intestine. Then he or she will sew the intestine back together.
The recovery and aftercare for each type of hernia repair is different. Your doctor or nurse can tell you what to expect after your surgery.
Component separation repair of large or complex abdominal wall defects
An increasing number of patients have large or complex abdominal wall defects. Such defects may result from incisional hernia related to multiple abdominal operations, surgical resection of the abdominal wall, necrotizing abdominal wall infections, or therapeutic open abdomen. The component separation technique, which was first described in 1990 for midline abdominal wall reconstruction, is a type of rectus abdominis muscle advancement flap that allows reconstruction of such large ventral defects. The advantages of the component separation technique are that it restores functional and structural integrity of the abdominal wall, provides stable soft tissue coverage, and optimizes aesthetic appearance.
INDICATIONS - Large or complex abdominal wall defects may be associated with problems such as chronic back pain, respiratory compromise, and altered body image. Patients with symptoms related to these defects or incisional hernias should ideally be repaired.
Large or complex abdominal wall defects are a particularly challenging surgical problem. Various methods of abdominal wall hernia repair (simple suture repair, mesh repair) using either open or laparoscopic approaches can be used to manage abdominal wall defects, which are most commonly related to incisional hernia.
The component separation technique, which was first described in 1990, is a very effective method for reconstructing large or complex midline abdominal wall defects in a manner that restores innervated muscle function without tension sometimes without the need for mesh.
Indications for a component separation technique include the following:
The component separation technique can restore abdominal wall functionality for defects up to 20 cm at the level of the umbilicus. In some patients with extremely large defects, the component separation technique alone may not allow restoration of the abdominal wall without tension. If the defect is too large to allow the flaps to be brought together at the midline, supplemental mesh can be used to bridge the residual defect.
The term acute abdomen represents the rapid onset of severe symptoms that may indicate potentially life-threatening intra-abdominal pathology that requires urgent surgical assessmnet and sometimes intervention. Abdominal pain is usually a feature, but a pain-free acute abdomen can occur, particularly in older people, in children, in the immunocompromised, and in the last trimester of pregnancy.
Acute abdominal pain is a frequent emergency department presentation. Pain may be located in any quadrant of the abdomen and may be intermittent, sharp or dull, achy or piercing; it may radiate from a focal site and there may be associated symptoms such as nausea and vomiting. Immediate assessment should focus on distinguishing those cases of true acute abdomen that require urgent surgical intervention from those that do not, which can initially be managed conservatively. Data from the UK suggest that availability and/or access to an experienced surgeon reduces unnecessary admissions while appropriately managing or triaging patients.
The Most Common causes of Acute Abdomen are:
1 Adhesions
2 Incarcerated/strangulated hernia
3 Cholecystitis
4 Gastric ulcer
5 Appendicitis
6 Ectopic pregnancy
7 Pelvic inflammatory disease
8 Acute pancreatitis
9 Acute diverticulitis
10 Ulcerative colitis
11 Crohn's disease
12 Cholelithiasis
13 Gastrointestinal malignancy
14 Hepatic abscess
15 Fitz-Hugh Curtis syndrome
16 Mallory-Weiss tear
17 Abdominal wall haematoma
18 Hereditary Mediterranean fever
19 Typhilitis (neutropenic enterocolitis)
20 Narcotic withdrawal
21 Hepatitis
22 Gastroenteritis
23 Infectious colitis
24 Sickle cell crisis
25 Endometriosis
26 Testicular torsion
27 Kidney stones
28 Pyelonephritis
Emergency Surgery can be defined as surgery that is required to deal with an acute threat to life, organ, limb or tissue caused by external trauma, acute disease process, acute exacerbation of a chronic disease process, or complication of a surgical or other interventional procedure. The skills needed for emergency surgery include the ability to diagmoses appropriately and undertake those abdominal and soft tissue procedures that need to be performed within appropriate time.
A diverticulum is a pouch-like structure that can form through points of weakness in the muscular wall of the colon (ie, at points where blood vessels pass through the wall).
Diverticulosis affects men and women equally. The risk of diverticular disease increases with age. It occurs throughout the world but is seen more commonly in developed countries.
What causes diverticular disease?
Diverticulosis — Diverticulosis merely describes the presence of diverticula. Diverticulosis is often found during a test done for other reasons, such as flexible sigmoidoscopy, colonoscopy, or CT Colonography. Most people with diverticulosis have no symptoms and will remain symptom free for the rest of their lives.
A person with diverticulosis may have diverticulitis, or diverticular bleeding.
Diverticulitis — Inflammation of a diverticulum (diverticulitis) occurs when there is thinning and breakdown of the diverticular wall. This may be caused by increased pressure within the colon or by hardened particles of stool, which can become lodged within the diverticulum.
The symptoms of diverticulitis depend upon the degree of inflammation present. The most common symptom is pain in the left lower abdomen. Other symptoms can include nausea and vomiting, constipation, diarrhea, and urinary symptoms such as pain or burning when urinating or the frequent need to urinate.
Simple diverticulitis, which accounts for 75 percent of cases, is not associated with complications and typically responds to medical treatment without surgery.
Complicated diverticulitis occurs in 25 percent of cases and usually requires surgery. Complications associated with diverticulitis can include the following:
• Abscess: a localized collection of pus
• Fistula: an abnormal tract between two areas that are not normally connected (eg, bowel and bladder)
• Obstruction: a blockage of the colon
• Peritonitis: infection involving the space around the abdominal organ
• Sepsis: overwhelming body-wide infection that can lead to failure of multiple organs
When to suspect diverticulosis
Diverticulosis is often found during tests performed for other reasons.
Barium enema – This is an x-ray study that uses barium in an enema to view the outline of the lower intestinal tract. This is an older test and has been largely replaced by computed tomography (CT) scan.
Flexible sigmoidoscopy – This is an examination of the inside of the sigmoid colon with a thin, flexible tube that contains a camera.
Colonoscopy – This is an examination of the inside of the entire colon.
A CT scan is often used to diagnose diverticulitis and its complications. If diverticulitis (not just diverticulosis) is suspected, the above three tests should not be used because of the risk of perforation.
How diverticulae are treated
Diverticulosis — People with diverticulosis who do not have symptoms do not require treatment. However, most clinicians recommend increasing fiber in the diet, which can help to bulk the stools and possibly prevent the development of new diverticula, diverticulitis, or diverticular bleeding. Fiber is not proven to prevent these conditions in all patients but may help to control recurrent episodes in some. Fruits and vegetables are a good source of fiber. The fiber content of packaged foods can be calculated by reading the nutrition label
Diverticulitis — Treatment of diverticulitis depends upon how severe your symptoms are.
Home treatment — If you have mild symptoms of diverticulitis (mild abdominal pain, usually left lower abdomen), you can be treated at home with a clear liquid diet and oral antibiotics. However, if you develop one or more of the following signs or symptoms, you should seek immediate medical attention:
Temperature >100.1°F (38°C)
Worsening or severe abdominal pain
An inability to tolerate fluids
Hospital treatment — If you have moderate to severe symptoms, you may be hospitalized for treatment. During this time, you are not allowed to eat or drink; antibiotics and fluids are given into a vein.
If you develop an abscess of the colon, you may require drainage of the abscess (usually performed by placing a drainage tube across the abdominal wall) or by surgically opening the affected area.
Surgical treatment for diverticulosis/diverticulitis
Surgery — If you develop a generalized infection in the abdomen (peritonitis), you will usually require an emergency operation. A two-part operation may be necessary in some cases.
-The first operation involves removal of the diseased colon and creation of a colostomy. A colostomy is an opening between the colon and the skin, where a bag is attached to collect waste from the intestine. The lower end of the colon is temporarily sewed closed to allow it to heal .
Approximately three to six months later, a second operation is performed to reconnect the two parts of the colon and close the opening in the skin. You are then able to empty your bowels through the rectum. Sometimes patients require up to a year to recover from the first operation, depending on how sick they were.
In non-emergency situations, the diseased area of the colon can be removed and the two ends of the colon can be reconnected in one operation, without the need for a colostomy.
Surgery versus medical therapy — An operation to remove the diseased area of the colon may not be necessary if you improve with medical therapy. However, people who are treated with an operation are felt to be cured, since only 15 percent of people develop further diverticulosis after surgery and only 2 to 11 percent of people need further surgery.
Thus, surgery may be recommended for people with repeated attacks of diverticulitis or if there are severe or repeated episodes of bleeding. The decision depends in part upon your other medical conditions and ability to undergo surgery.
Some healthcare providers recommend surgery after the first attack of diverticulitis in people who are less than 40 to 50 years. The reason for this is that the disease may be more severe in this age group and there may be an increased risk of recurrent disease that will ultimately require surgery. Thus, having surgery at a young age could potentially eliminate the chances of developing worsened disease. The decision to undergo surgery ultimately depends upon your surgeon's recommendations.
In many cases, an elective operation can be performed laparoscopically, using small incisions, rather than the typical vertical (up and down) abdominal incision. Laparoscopic surgery usually allows you to recover more quickly and shortens the hospital stay.
Recovery from diverticulitis — After an episode of diverticulitis resolves, if you have not had a recent colonoscopy, the entire length of the colon should be evaluated to determine the extent of disease and to rule out the presence of abnormal lesions such as polyps or cancer. Recommended tests include colonoscopy, barium enema and sigmoidoscopy, or CT colonography.
Diverticular bleeding Most cases of diverticular bleeding resolve on their own. However, some people will need further testing or treatment to stop bleeding, which may include a colonoscopy, angiography (a treatment that blocks off the bleeding artery), bleeding scan, or surgery.
Diverticular colitis Patients with diverticular disease can develop a segmental colitis most commonly in the sigmoid colon. Segmental colitis associated with diverticula (SCAD) or diverticular colitis is characterized by inflammation in the interdiverticular mucosa without involvement of the diverticular orifices. Patients with segmental colitis associated with diverticulosis (SCAD) typically present with chronic diarrhea, cramping abdominal pain primarily in the left lower quadrant, and in some cases intermittent hematochezia The optimal treatment of segmental colitis associated with diverticulosis (SCAD) has not been well defined and different treatment regime includes Anthibiotics and Luminal antiinflammatory.
| Treatment | Dose |
|---|---|
| Venalex | 1000mg |
| Levorag | 250mg |
| Fleben | 1000mg |
Colorectal cancer, also known as bowel cancer, colon cancer or rectal cancer is any cancer (a growth, lump or a tumour) of the colon and the rectum. The World Health Organization and CDC say it is the second most common cancer worldwide, after lung cancer.
Symptoms of colorectal cancer
Going to the toilet more often
Diarrhoea
Constipation
A feeling that the bowel does not empty properly after a bowel movement
Blood in feces (stools)
Pains in the abdomen
Bloating in the abdomen
A feeling of fullness in the abdomen (maybe even after not eating for a while)
Vomiting
Fatigue (tiredness)
Inexplicable weight loss
A lump in the tummy or a lump in the back passage felt by your doctor
Unexplained iron deficiency in men, or in women after the menopause
Small bowel cancer starts when healthy cells in the lining of the small bowel change and grow out of control, forming a mass called a tumor. A tumor can be cancerous or benign. A cancerous tumor is malignant, meaning it can grow and spread to other parts of the body. A benign tumor means the tumor can grow but will not spread. These changes can take a long time to develop. Both genetic and environmental factors can cause such changes, although the specific causes of small bowel cancer are generally not well understood.
Types of small bowel cancer
There are 5 main types of small bowel cancer:
Adenocarcinoma
Adenocarcinoma is the most common type of small bowel cancer, usually occurring in the duodenum or jejunum. Adenocarcinoma begins in the gland cells of the small bowel.
Sarcoma
Small bowel sarcoma is generally a leiomyosarcoma, which is a tumor that arises in the muscle tissue that makes up part of the intestine. This type of tumor most often occurs in the ileum. Learn more about sarcoma.
Gastrointestinal stromal tumor (GIST)
GIST is an uncommon tumor that is believed to start in cells found in the walls of the gastrointestinal (GI) tract, called interstitial cells of Cajal (ICC). GIST belongs to a group of cancers called soft tissue sarcomas. Learn more about gastrointestinal stromal tumors.
Carcinoid tumor
Carcinoid tumors are classified as neuroendocrine tumors. These are tumors that start in the hormone-producing cells of various organs and generally occur in the ileum. Learn more about carcinoid tumors.
Lymphoma
Lymphoma is a cancer of the lymph system, which is part of the body’s immune system. Lymphoma that occurs in the small bowel usually occurs in the jejunum or ileum and is most commonly non-Hodgkin lymphoma. Learn more about non-Hodgkin lymphoma.
Proctology is the medical speciality in the diagnosis of disease, prevention and treatment of the anus and rectum, otherwise known as anorectal problems.
An anal abscess is an infected cavity filled with pus near the anus or rectum.
An anal fistula (also called fistula-in-ano) is a small tunnel that tracks from an opening inside the anal canal to an outside opening in the skin near the anus. An anal fistula often results from a previous or current anal abscess. As many as 50% of people with an abscess get a fistula. However, a fistula can also occur without an abscess.
Small glands just inside the anus are part of normal anatomy. If the glands in the anus become blocked, this may result in an infection. When the infection is serious, this often leads to an abscess. Bacteria, feces, or foreign matter can also clog the anal glands and cause an abscess to form. Crohn’s disease, cancer, trauma and radiation can increase the risk of infections and fistulas.
A patient with an abscess may have pain, redness or swelling in the area around the anal area or canal. Other common signs include feeling ill or tired, fever and chills. Patients with fistulas have similar symptoms, as well as drainage from an opening near the anus. A fistula is suspected if these symptoms tend to keep coming back in the same area every few weeks.
Most anal abscesses or fistulas are diagnosed and managed based on clinical findings. Occasionally, imaging studies such as ultrasound, CT scan or MRI can help in the diagnosis and management of deeper abscesses and may be used to visualize the fistula tunnel.
The treatment of an abscess is surgical drainage under most circumstances. It is important that your surgeon be very familiar with treating abscesses and fistula. Colorectal surgeons are experts in this area. For most patients, an abscess can be drained surgically through a simple procedure. An incision is made in the skin near the anus to drain the infection. Some patients with more severe disease may require multiple surgeries to take care of the problem.
Surgery is nearly always needed to treat an anal fistula. In many patients, if the fistula is not too deep, a fistulotomy is performed. During this surgery, the fistula track will be opened to allow healing from the bottom up. The surgery may require dividing a small portion of the sphincter muscle. A large amount of the sphincter muscle is not divided as this could lead to problems with bowel control (fecal incontinence) in some patients. If the fistula track does involve a large portion of the sphincter muscle, other more involved surgeries are done to treat the fistula without harming the sphincter muscle. More difficult cases may require multiple surgeries.
Antibiotics alone are not effective in treating abscesses or fistula. Antibiotics may be needed, in addition to surgery, if a patient has immunity issues, specific heart valve conditions or widespread cellulitis (a bacterial infection of the skin and tissues under the skin). Providing your physician with an accurate medical history and undergoing a physical exam are important steps in deciding if antibiotics are required.
An anal fissure is a small tear in the skin around the opening of the anus (the end of the back passage). The symptoms of anal fissures are:
Anal fissures can occur at any age but are seen more in young adults between the ages of 20-40. They affect both men and women equally and can occur in childhood
The most common cause of an anal fissure is constipation and passing hard stool, which can damage the lining of the anal canal.
Other causes may be persistent diarrhoea, passing loose stools frequently, childbirth and inflammatory bowel disease
If you see blood in your stool or any other symptoms of an anal fissure you should visit your GP.
Anal fissures usually heal within a few weeks without any need for medical treatment, but this is not the case for everyone. One common problem is that severe pain may cause people to avoid passing stools, triggering the symptoms of constipation, which may prevent the fissure from healing and lead to chronic anal fissures. Switching to a high fibre diet should help recovery by making it easier to pass stools.
While many anal fissures will heal by themselves, some may require medication. There are a number of treatments that will help the fissure to heal, as well as ease the symptoms.
Softening stools: This allows stool to pass more easily, reducing pain and aiding the healing process. This can be done by increasing the amount of fibre in the diet or through medications called laxatives. These will help your stools retain water, which will make them softer and more bulky.
Medications:
Topical (medicine that you apply directly onto the affected body part) anaesthetics such as lidocaine could be used to numb the area and ease the pain.
Topical Glyceryl Trinitrate 0.2-0.4 %(GTN) is another treatment that can be used if symptoms do not improve, which acts to increase blood flow by expanding nearby vessels, which can help the fissure to heal.
Topical Diltiazem Cream 2% It increases blood flows to smooth muscles and relaxes muscle tone. Topical diltiazem hydrochloride is not licensed in the UK for treating chronic anal fissure or any other indication. Therefore, its use for treating chronic anal fissure is unlicensed.
Botulinum toxin (BTX) can be used for temporary chemical denervation to treat this painful disorder. Its application is by intramuscular injections into either the external or internal anal sphincter muscle. The healing rate is dependent on the BTX dosage. The short-term healing rate (≤ 6 months) is 60–90%, whereas about 50% of the patients show a complete response in long-term follow-up studies (> 1 year).
THD Levorag(®) Emulgel proved to be effective for the re-epithelization of AF and the reduction of pain in the short term in about 80 % of patients. Its use for treating anal fissure is unlicensed a recent trial has demonstrated good results compared with routine treatment and the medication can be purchase from: levorag.co.uk
If the fissure does not respond to treatment then you may be referred for further treatment, which could involve some form of surgery. The most common type of surgery used is called advancement flap and internal sphincterotomy. This involves a general anaesthetic and can often be done without requiring an overnight stay in hospital, but can, very rarely, lead to permanent incontinence. Your doctor will explain the options available to you and the risks involved,
Fissures can reappear and a fully healed fissure may come back if a hard stool is passed, which causes further damage. One of the best ways to prevent fissures returning is to avoid becoming constipated. Some methods to prevent constipation are:
Haemorrhoids are a result of the inflammation of veins supplying the rectum, anal canal and low rectum.
There are two types:What is pilonidal sinus and who gets it?
A pilonidal sinus is a small tunnel/cavity in the skin, which is usually found at the top of the cleft between the buttocks. The cavity can become infected causing symptoms such as pain, swelling and the development of a pus-filled abscess within the sinus. If the sinus becomes infected it should be treated to prevent the infection from spreading and further complications occurring.
Who gets pilonidal sinuses?
Each year pilonidal sinuses affect around 26 in 100,000 people in the UK. It is more common in men than women and typically affects young people between puberty and the age of 40.
Risk factors and causes
Factors which increase the risk of a pilonidal sinus developing include:
What causes a pilonidal sinus?
The exact cause of pilonidal sinuses remains unclear but there are various theories used to help explain how they may occur. The underlying issue seems to be penetration of loose hairs into the skin or the blockage of a hair follicle. The area becomes inflamed and a bacterial infection is then likely to occur due to the warm and moist nature of the cleft between the buttocks.
Pressure or trauma at the affected area can cause further irritation and encourage more hair or debris to collect within the sinus. The area may become chronically inflamed/ infected with multiple sinuses joining together.
Symptoms
You may not have symptoms, although you may notice a small dimple (sometimes more than one) or depression in your skin. However, if the sinus becomes infected, you may experience symptoms such as:
Treatment
ACUTE ABSCESS
An acute pilonidal abscess is managed with an incision and drainage (I&D) procedure at the time of presentation, usually under local or general anesthesia. This management approach is consistent with simple incision and drainage of pus. Wounds are packed with gauze, and healing occurs by secondary intention in the acute setting. An I&D, however, is not the definitive procedure for pilonidal disease, as recurrence rates range from approximately 20 to 55 %.
CHRONIC OR RECURRENT DISEASE
The definitive treatment of chronic or persistent pilonidal disease is a surgical excision of all sinus tracts . The surgical procedures range from simple excision with or without primary closure to complex flap reconstruction.
Recurrence rate — Based upon research, the overall recurrence rate of pilonidal disease is 6.9 percent. Primary wound closure is associated with a significantly higher recurrence rate compared with a delayed wound closure (8.7 % versus 5.3 %)
Surgical site infections — Overall, surgical site infections (SSI) is between 8 to 10%.
Time to return to work — Patients undergoing a primary repair had a significantly faster rate of return to work compared with patients with open wounds (12 versus 18 days)
Pruritus Ani is the medical term for intense itching around the anus that leads to the strong urge to scratch the bottom. Up to 5% of the population is estimated to be affected and the condition is more common in men than in women.
There are many possible causes of Pruritus Ani.
One cause is incontinence of stool. This can be due to loose stools and diarrhoea or amounts of stool so small that they are undetectable. Itching is also commonly associated with other conditions such as haemorrhoids, anal fissures and anal fistulas. Bacterial and fungal infections are responsible for some cases of pruritus ani. Some of these infections can be transmitted sexually. Some medications such as steroid creams, antibiotics and some haemorrhoid treatments can cause or worsen symptoms.
Pruritus ani may be associated with skin conditions such as psoriasis and contact dermatitis. Contact dermatitis is skin that is very sensitive to chemicals found in cleansing products such as soap. Common conditions such as diabetes, anaemia, kidney and thyroid disorders can also cause itching. Very rarely and itchy bottom can be caused by a cancer of the skin around the anus.
Some foods and drinks such as tomatoes, chocolate, citrus fruits, spices, coffee, tea, alcohol and milk are known to cause itching in some people. In others, itching can be precipitated by stress, anxiety and depression.
In some cases no cause can be identified. This is called idiopathic pruritus ani.
If you are experiencing itching around the anus, it is recommended that you see your GP to find out the underlying cause and to exclude any other conditions.
Your GP will ask you several questions to find out more about your symptoms. This is likely to include questions about your diet, bowel habit, personal hygiene, sexual history and other genital symptoms that will help your doctor reach a diagnosis.
The GP is likely to want to examine your bottom. As well as inspecting the skin around the anus, an examination of the genitals is useful to identify anything that you have not yet noticed. The doctor may perform a digital rectal examination which involves placing a gloved and lubricated finger inside the rectum to look for things that may be causing the itching. This should not be painful but may feel uncomfortable. At this point swabs may be taken to check for infection.
For those cases of Pruritus Ani with an underlying cause, the goal is to find this cause and treat it. This may require referral to a specialist dermatologist for those with suspected skin conditions or a colorectal surgeon for those with suspected ano-rectal disease.
For some people in whom a cause is not identified. Lifestyle changes are recommended to stop or improve symptoms. These include:
Keeping the area clean and dry. Have a bath or shower daily. After passing stools, clean the area with lukewarm water using a wet cloth, shower or bidet. Do not use soap antiseptics or scented products on your bottom. Dry by gently patting a soft cloth, unbleached toilet paper or by using a hairdryer on a low setting. Wearing loose cotton underwear is recommended.
Dietary changes are often necessary for treatment. There are several common foods which may be related to pruritus ani. These foods and beverages include coffee, colas, tea, chocolate, tomatoes and beer. These items may possibly decrease your sphincter tone which can cause some seepage or leakage.
It may be helpful to remove one item at a time from your diet for several weeks. If your symptoms improve, you could try reintroduction of the item in smaller volume and see if there is a limit to which you may have that item without producing symptoms.
Improving the consistency of stools by altering fibre and fluid intake.
Avoid scratching although this may be very difficult. Prevent inadvertent night time scratching by keeping fingernails short or wearing gloves to bed.
A skin barrier cream such as zinc oxide may also be helpful in protecting the skin around the anus from irritants. Additional topical agents such as numbing medications, menthol, phenol, camphor, or a combination of them may be helpful.
Your doctor may prescribe creams or ointments containing steroids or other substances. This will improve symptoms for most people. If this is not the case, make sure you inform your doctor.
Rectal prolapse in adults is a rare condition that happens when some or all of the tissue that lines the rectum sticks out of the anus. It is most common in older women but can happen in men and women of all ages.
Women who have had more than one baby delivered through the vagina are more likely to get rectal prolapse. Other health conditions that can make rectal prolapse more likely include:
Long-term bowel problems such as:
Constipation - This means your bowel movements are too hard or small, difficult to get out, and happen fewer than 3 times per week.
Straining during bowel movements
Diarrhoea – This means your bowel movements are watery or runny and happen more than 3 times a day.
Problems in the pelvic area, including weak muscles or a history of pelvic surgery.
The main symptom is bright red tissue sticking out of the anus. The tissue might have mucus or blood on it. Rectal prolapse is not usually painful but can be uncomfortable. The tissue might stay outside the anus or move back inside the body.
Other symptoms include:
Trouble starting a bowel movement
Feeling like you have not fully emptied your bowels
Leaking solid or liquid bowel movements (called "fecal incontinence")
The treatment depends on how serious your symptoms are and if you have other health problems. Whatever treatment you have, your doctor will likely tell you to:
Eat foods that have a lot of fiber. Good choices are fruits, vegetables, prune juice, and cereals. You should eat between 25 to 30 grams of fiber per day.
Drink 4 to 8 cups of water or other fluids per day.
Other treatments include:
Laxatives - These are medicines that help make bowel movements easier to get out. Some are pills that you swallow. Others go into the rectum and are called "suppositories."
Enemas - For this treatment, a doctor or nurse squirts fluid into your rectum to help empty your bowels.
Pelvic floor exercises with biofeedback – These exercises strengthen the muscles that control the flow of urine and bowel movements.
Doctors use different kinds of surgery to fix rectal prolapse. The surgery is done either through the belly (Rectopexy) or in some cases; it is done through the area between the genitals and the anus, called the "perineum." (perineal rectosigmoidectomy and delorme procedure)